Medical Coding Pro - Protect Incident To Pay
Published: Thu, 08/12/10
As a benefit for being on our mailing list we are sending out a
weekly update including links to the most recent posts on our
blog. If you would like to read further just click one of the links.
Kind Regards,
The Medical Coding Pro Team
Great Deal On Practice Exams
http://www.medicalcodingpro.com/store.html
Medical Coding Pro
Coders Destination for Information
http://medicalcodingpro.com/wordpress
Protect Incident To Pay - 2010-08-12 11:27:41-04
Incident-to services are on auditors radar. To prevent paybacks, you’ve got to know when to use incident to – and capture full pay, and when to bill services directly – and lose the standard 15%. Test your incident to savvy with this question: Qu...
Read more: http://medicalcodingpro.com/wordpress/archives/1116
Watch for Denials If You Take Shortcuts on Form 5010 - 2010-08-12 11:34:53-04
 Say goodbye to form 4010A1 for ICD codes as well, starting in 2012.
Say goodbye to form 4010A1 for ICD codes as well, starting in 2012.
Dig into your claim forms now to ensure that the beneficiary’s information is accurate to the letter, or you’ll face scores of denied claims on the new HIPAA 5010 forms.
Why it matters: CMS will deny claims on which the beneficiary’s name doesn’t perfectly match how it’s listed on his Medicare I.D. card when you begin using HIPAA 5010 form — the new Medicare universal claim form starting in 2012.
Include Jr. or Sr. Suffixes
“Whenever there is a name suffix, such as ‘Jr.’ or ‘Sr.’ abbreviations, etc., it must be included with the last name,” said Veronica Harshman of CMS’s Division of Medicare Billing Procedures during an April 28 Open Door Forum regarding the eligibility component of the HIPAA 5010 form.
You can include the suffix either with the patient’s last name or in the suffix field, specified CMS’s Chris Stahlecker during the call.
“The date of birth must also match exactly to what the Social Security Administration has on file,” Harshman said. CMS will use several new error codes on claims once the 5010 form goes into effect. “If you communicate with CMS through a third-party vendor (clearinghouse), it is strongly recommended that you discuss with them how these errors will be communicated to you and how these changes will impact you and your business,” Harshman advised.
Look for Production Systems Next Year
According to the HIPAA 5010 Final Rule, CMS will have a production 5010 system available as of Jan. 1, 2011, Harshman said.
The last day CMS will accept a 4010A1 form will be Dec. 31, 2011. As of Jan. 1, 2012, if you aren’t using the 5010 form, you’ll “lose the ability to receive eligibility data from Medicare,” Harshman said. In...
Read more: http://medicalcodingpro.com/wordpress/archives/1115
CCI 16.2 Bundles Paravertebral Facets With Anesthesia Procedures - 2010-08-12 16:17:13-04
Don’t assume separate coding for J0670, anymore.
The latest Correct Coding Initiative (CCI) edits contain plenty of anesthesia and pain management pairs you should check — and straight away. They went into effect July 1. CCI 16.2 encompasses 16,843 new edit pairs, according to analyst Frank Cohen, MPA, of MIT Solutions, Inc., in Clearwater, Fla. With 11 percent of all active edits affecting anesthesia procedures, you can’t afford to miss any of the changes.
Other Work Includes Paravertebral Facet Injection
Although the current CPT book doesn’t include them, you could begin using several new codes for paravertebral facet joint injections in January 2010. Now CCI edits bundle two of the new codes with every anesthesia code (00100-01999) and many nerve destruction procedures. The paravertebral injection codes affected are:
- 0213T — Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, cervical or thoracic; single level
- 0216T — Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, lumbar or sacral; single level.
Procedures paired with 0213T and 0216T range from 64600 (Destruction by neurolytic agent, trigeminal nerve; supraorbital, infraorbital, mental, or inferior alveolar branch) and 64622 (Destruction by neurolytic agent, paravertebral facet joint nerve; lumbar or sacral, single level) to 64650 (Chemodenervation of eccrine glands; both axillae). Most of the edit pairs carry a “0” modifier indicator, but CCI lists a few with modifier indicator “1.” Check the full CCI file to verify whether you can use a modifier to break specific edits.
ME Edits Also Hit 0213T-0218T
Paravertebral facet joint injection codes 0213T-0218T come into play as part of mutually exclusive (ME) edits, as well.
CCI 16.2 pairs each choice with corresponding codes involving fluoroscopy or CT guidance: 64490-64492 (Injection[s], diagnostic or...
Read more: http://medicalcodingpro.com/wordpress/archives/1123
Medicare Repeat Pap Smears: Find Out If 99000 Is OK - 2010-08-12 16:23:22-04
Hint: Abnormal versus insufficient cells mean different diagnosis codes.
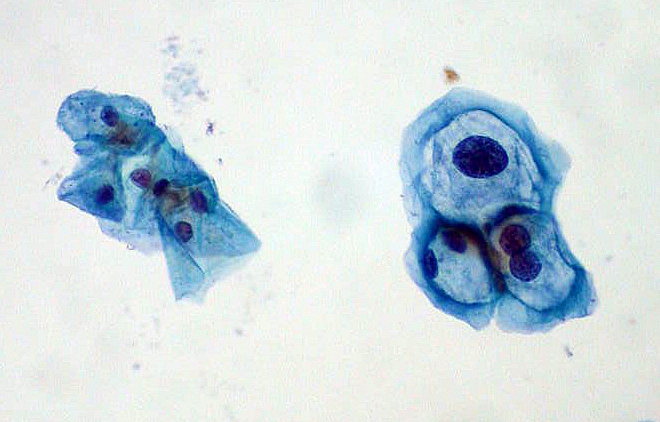 When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.
When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.
Question 1: When a patient comes in for a second Pap smear, what CPT code(s) should you apply and why?
Question 2: Will you receive reimbursement for handling the repeat Pap smear? Why or why not?
Question 3: If the patient comes back in for a Pap smear due to abnormal results, what ICD-9 code(s) should you use and why?
Question 4: If the patient has a repeat Pap because the lab did not have enough cells in the specimen to interpret the results, what ICD-9 code(s) should you use and why?
Answer 1: Here’s What CPT Codes
When the patient comes in for a second Pap smear, submit the appropriate E/M office visit code (99211-99215). You will probably be able to report 99212 (Office or other outpatient visit for the evaluation and management of an established patient …) for this visit because the patient likely will come in only for the Pap smear and CPT does not include a specific code for taking the Pap. Code 99212 carries 1.08 relative value units (RVUs), unadjusted for geography. That translates to about $31 for this visit (using the new conversion factor of 28.3868).
Answer 2: Handling the Specimen Depends on Payer
Some private payers will reimburse for handling the repeat Pap smear specimen (99000, Handling and/or conveyance of specimen for transfer from the physician’s office to a laboratory). But Medicare carriers consider the collection and handling part of...
Read more: http://medicalcodingpro.com/wordpress/archives/1122
ICD-9 2011 Diagnosis Coding: New Ectasia Codes Come Oct. 1 - 2010-08-12 16:26:34-04
 Check out V13.65 for corrected congenital heart malformations.
Check out V13.65 for corrected congenital heart malformations.
Each October you’re faced with new ICD-9 codes to add to your diagnosis arsenal. 2011 is no exception, with new ectasia, congenital malformation, and body mass index (BMI) codes you’ll need to learn. Take a look at the proposed changes that will affect your cardiology practice, so that you’re ready when fall rolls around.
End Your Ectasia Hunt at 447.7x
The proposed changes to ICD-9 2011 add four codes specific to aortic ectasia, which could be among the most significant changes for cardiology coders.
“Ectasia” means dilation or enlargement, and aortic ectasia often refers to an enlargement that is milder than an aneurysm. But ICD-9 2010 does not distinguish ectasia from aneurysm, linking aortic ectasia to 441.9 (Aortic aneurysm of unspecified site without mention of rupture) and 441.5 (Aortic aneurysm of unspecified site, ruptured).
The proposed 2011 codes are specific to aortic ectasia and are based on anatomic site:
- 447.70 — Aortic ectasia, unspecified site
- 447.71 — Thoracic aortic ectasia
- 447.72 — Abdominal aortic ectasia
- 447.73 — Thoracoabdominal aortic ectasia.
New Corrected Congenital Malformations Code
A number of new codes deal with congenital malformations of the heart and circulatory system. Code V13.65 (Personal history of [corrected] congenital malformations of heart and circulatory system) will be “very useful to our practice,” says Janel C. Peterson, CPC, with Alegent Health Clinic Heart and Vascular Specialists in Omaha, Neb.
Add BMI V Codes to Your E/M Arsenal
The ICD-9 proposal has “expanded the body mass index (BMI) codes to demonstrate higher BMIs with five new codes,” notes Barbara J. Cobuzzi, MBA, CPC, CPC-H, CPC-P, CENTC, CHCC, with CRN Healthcare Solutions in Tinton Falls, N.J.
You’ll need to stop using V85.4 (Body Mass Index 40 and over, adult) on Oct. 1 and start...
Read more: http://medicalcodingpro.com/wordpress/archives/1121